This is Naked Capitalism fundraising week. 659 donors have already invested in our efforts to combat corruption and predatory conduct, particularly in the financial realm. Please join us and participate via our donation page, which shows how to give via check, credit card, debit card, or PayPal. Read about why we’re doing this fundraiser, what we’ve accomplished in the last year,, and our current goal, rewarding our guest bloggers.
By Lambert Strether of Corrente.
What is infection control? According to the CDC:
Infection control prevents or stops the spread of infections in healthcare settings.
Which, arguably, hospitals are. In fact, hospitals have administrative structures for Hospital Infection Control (HIC). Again the CDC:
The role of the hospital infection control committee (HICC) is to implement the annual infection control programme and policies….
- Develop a system for identifying, reporting, analyzing, investigatingand controlling HCAIs
- Develop and implement preventive and corrective programs in specific situations where infection hazards exist….
- Review and update hospital infection control policies and proceduresfrom time to time.
HICC shall meet regularly – once a month and as often as required.
Since we’re now 924 days / 30 = ~30 months = 30 meetings into the latest Coronavirus pandemic, one would have expected those regular monthly meetings to have culminated in robust and coherent “politicies and procedures” to prevent the airborne transmission[1] of SARS-CoV2. But who am I kidding? Nothing could be further from the truth.
Here are some revealing anecdotes[2]. (I’m including medical offices because the hospitals are the hegemonic institution in the delivery of health care in the United States, and others could be expected to follow their lead.) For example:
I’m in a hospital right now in Iowa astounded that masks are no longer required. Absolutely bonkers.
— Snickademous (@Snickademous) September 7, 2022
And:
Why am I in a hospital and no one is wearing masks
— Jessica (@jes_klein_) September 8, 2022
Day 2: no masks I’m going to die here
— Jessica (@jes_klein_) September 9, 2022
And:
It does. Was recently in Pennsylvania at a hospital and no masks required. At home in New Jersey, masks required in ALL medical facilities
— Lucy🐾💚 Sadie🐾💛 & Mom 🦄💙 (@corganddox1215) September 10, 2022
And:
My 73 year old brother went by ambulance to an ER in IA cuz he couldn’t breathe. He tested Covid+ & has pneumonia. He was wearing a mask when he got there & staff told him he didn’t have to, IN A HOSPITAL ER! He said one Dr was masked, but no one else. WTH is going on?
— chicky ✍🏻 (@_chicky_little) September 10, 2022
And:
Urgent care last Monday for abdominal pain. Masks optional, people coughing in the waiting room. Wearing my n95. Mammogram today, masks optional in the hospital system. Tech wore a surgical. I was in an n95. Potentially risking my health for urgent and preventative care.
— njphlaz 🐝👩🔬 (@njphlaz) September 9, 2022
And finally:
Dr appt. today, large medical building, lots of dr. offices. Not a single mask on anyone, including my dr and his nurses. I wore my mask.
— Leah Hamilton (@LeaHami55821459) September 10, 2022
At the very least, mask policy — the first layer of defense against aerosol transmission, before ventilation — is inconsistent (or inconsistently enforced) across jurisdictions in hospitals. So it’s no wonder that Politico writes “Nowhere is safe: Record number of patients contracted Covid in the hospital in January“[3]:
More than 3,000 hospitalized patients each week in January had caught Covid sometime during their stay, more than any point of the pandemic, according to U.S. government data analyzed by POLITICO.
The record surge demonstrates the virulence of the Omicron variant and how even hospitals, where infection control is paramount, provided little refuge.
“Any level of hospital transmission is concerning,’ said Aaron Milstone, a professor at the Johns Hopkins Bloomberg School of Public Health who focuses on the prevention of hospital-acquired infections. .”
(lol no.) This article appeared in February, 2022. Six HICC meetings later, nothing has changed. Interestingly, the issue of whether Covid is airborne and if so, what practices to adopt, blew up way back in 2020. From KHN via the Guardian:
Frontline healthcare workers are locked in a heated dispute with many infection control specialists and hospital administrators over how the novel coronavirus is spread – and therefore, what level of protective gear is appropriate.
At issue is the degree to which the virus is airborne – capable of spreading through tiny particles lingering in the air – or primarily transmitted through large, faster-falling droplets from, say, a sneeze or cough. This wonky, seemingly semantic debate has a real-world impact on what sort of protective measures healthcare companies need to take to protect patients and their workers.
In fact, the administrators and the infection control specialists won (as we see from the anecdotes and data above). (See, .e.g., “Some hospitals ask patients, visitors to remove N95s, citing CDC.”) Why?
In this post, I will show that CDC — hold onto your hats, here, folks — rejects airborne tranmission for Hospital Infection Control[4], indeed for Covid. I will then present new data that shows how airborne transmission is pervasive in hospitals, reinforcing the data and anecdotes given above. I will conclude by speculating why CDC is so sickeningly derelict in its mission to “fight disease and support communities and citizens to do the same.” This is especially unfortunate, since the CDC created the field:
Infection control (now infection prevention) in healthcare settings is a relatively young medical discipline dating back only to the 1970s. Nationwide surveillance for healthcare-associated infections (HAIs) was initiated by the Centers for Disease Control and Prevention (CDC) in 1970 via the National Nosocomial Infections Study (NNIS).
Tne CDC Infection Control Documentation Rejects Aerosol Transmission
I’m going to take a short journey through the CDC’s “Infection Control” page, looking for what it has to say about airborne transmission. There is a table of contents at too right; I’ve highlighted the areas I am going to look at:
The “How Infections Spread” page has a cute little three-tab widget under the heading “How Do Infections Occur?”. The tabs are “Source,” “Susceptible Person,” and “Transmission.” Let’s look at each tab in turn.
Source;
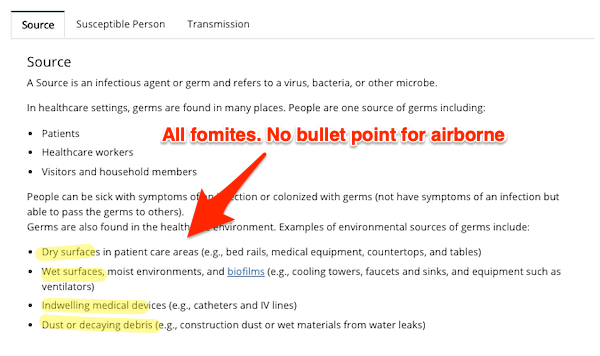
As you can see, this page has bullet points for examples of transmission via fomites, but there is nothing specific for airborne. Yes, “people are one source of germs,” but there is no indication of how or why. One might imagine a bullet point for, say, breathing (which creates shared air). But no.
Susceptible Person:
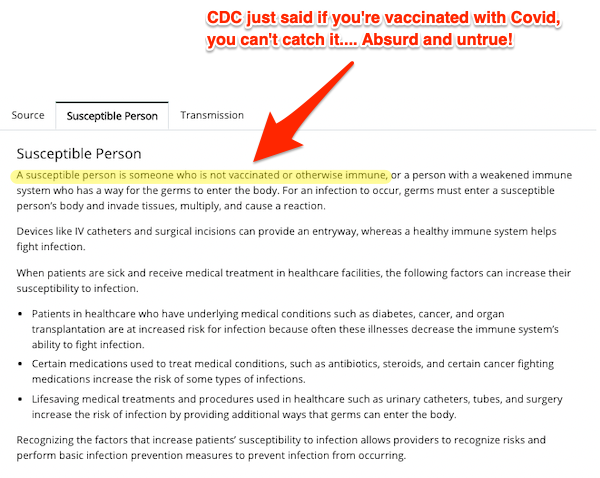
This page contains, at least for Covid, an outright falsehood. Plenty of people who have been vaccinated are “susceptible” to Covid.
Transmission:
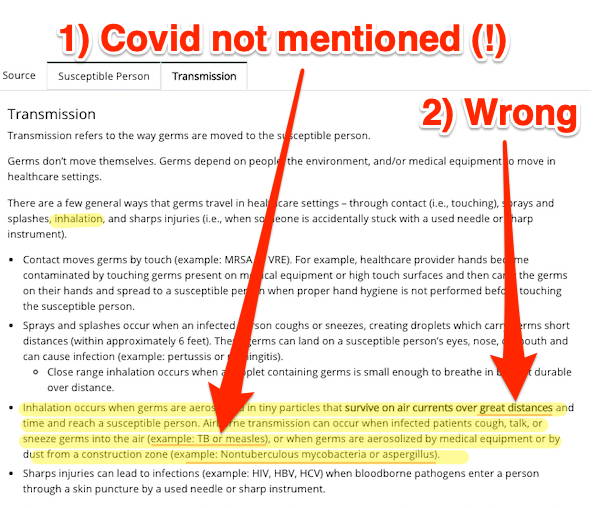
Here, finally, we get a mention for airborne transmission (although one would have expected people to have been given as an example on page one). However, 1) and jaw-droppingly, Covid is not mentioned (which would lead an innocent reader to assume that Covid was not airborne). And 2) aerosol transmission is not confined to “long distance” infection [pounds head on desk]. If you’re sharing air with an infected person, that person can be six inches, six feet, or six yards away (the latter two depending on the quality of ventilation).
Now we turn to the “Infection Control Basics” page. There are two sections: “Standard Precautions for All Patient Care”, and “Transmission-Based Precautions”:
Standard Precautions for All Patient Care:
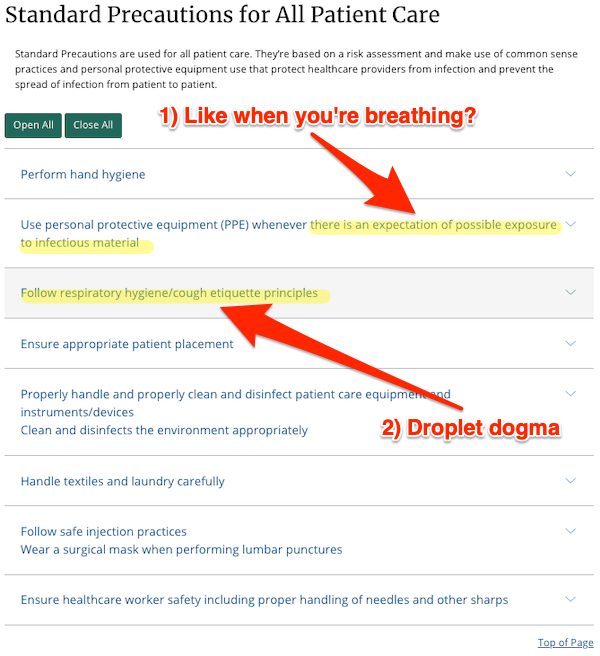
As I shall show below, 1) the possibility of Covid infection in hospitals is pervasive. Hence, the concept that there are some spaces where PPE is appropriate, and some where it is not, is wrong. “Respiratory Hygiene/cough etiquette” 2) is droplet dogma; it ignores airborne transmission via breathing, talking, singing, etc.
Transmission-Based Precautions
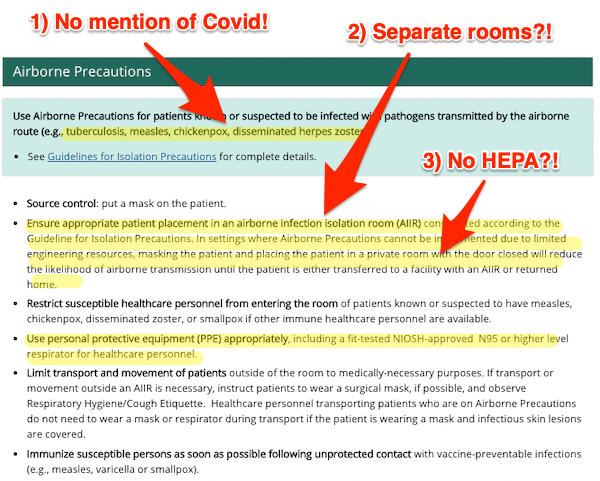
Once again, 1) there is no mention of Covid. A reasonable reader, considering the salience of Covid on the nightly news or in professional literature, would conclude that Covid is not airborne. 2) The idea that infectious/susceptible persons should be given separate rooms flies in the face that the fact that airborne Covid is pervasive in the hospital setting. Meanwhile, the idea that one might 3) place them in a separate room, but without a HEPA filter, is absurd.
Finally, we turn to the page for “Tools for Healthcare Settings.” (If you go to the link, you will see that there is nothing specific for airborne transmission)
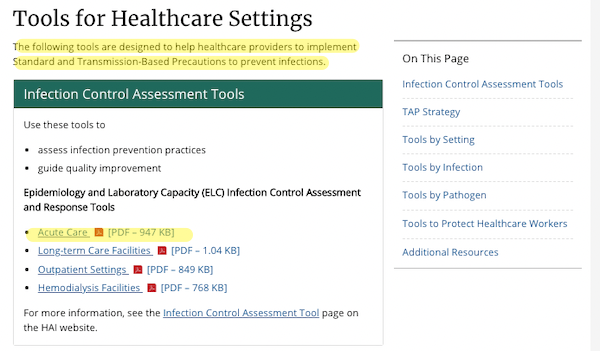
I will look at the “tool” for “Acute Care,” which I take to cover hospitals.The “tool” is in fact a ginormous survey instrument (PDF). Here is the heading:
“Assist in the assessment of infection control programs” this “tool” certainly does. But I can assure you that there are no entries for “ventilation,” “HEPA,” or anything useful for “air.”
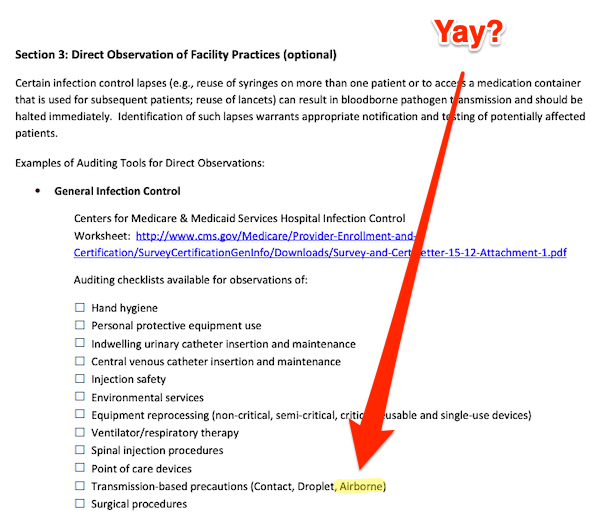
There is an optional section that mentions “airborne,” I suppose on the assumption that only some facilities have issues with airborne transmission of Covid:
So I clicked through to the link given, and found a “Hospital Infection Control Worksheet” from CMMS. Here is the first page, but the rest has the same assumptions:
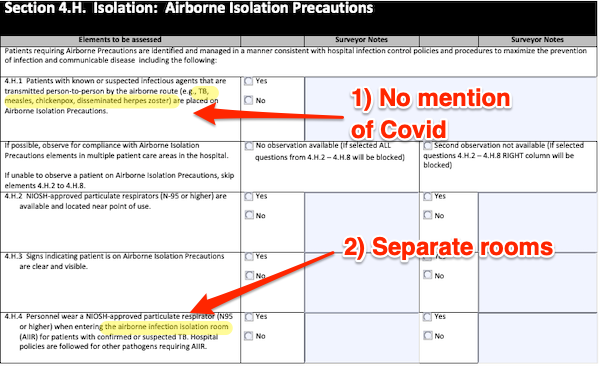
So we find the same weaknesses as in “Transmission-Based Precautions” above. 1) Covid is not mentioned. 2) Infectious Persons are to be placed in AIIRs (Airborne Isolation Infection Rooms) in which, in section 4.H.6 on the next page, and contradicting earlier guidance, HEPA filters are mandated, just not for everyone else. So there’s no thought of HEPA filters anywhere else, like ordinary rooms, or waiting rooms, or offices.
A reasonable person would conclude from reading this checklist that if a hospital can isolate measles patients, it can handle airborne transmission in the general case. Not so!
So if you’re looking for a reason why HICCs keep meeting, month after month, and not accepting that Covid is airborne, or doing anything about it, it’s because their hegemonic authority on infection control, CDC, hasn’t given them any reason to believe otherwise. For starters.
Airborne Transmission of Covid is Pervasive in Hospitals
From the preprint “The aerobiology of SARS-CoV-2 in UK hospitals and the impact of aerosol generating procedures“:
Aerosol generating procedures (AGPs) seemed particularly risky, and policies have restricted their use in all settings. We examined the prevalence of aerosolized SARS-CoV-2 in the rooms of COVID-19 patients requiring AGP or supplemental oxygen compared to those on room air.
(An example of an AGP is a tracheotomy. AGPs are the only form of aersols in hospitals that “droplet dogma” permits.) From samples in 219 rooms, ” the largest air sampling study for SARS-Cov-2 published to date”:
SARS-CoV-2 viral RNA was detected in the air of hospital rooms of COVID-19 patients, and AGPs did not appear to impact the likelihood of viral RNA. Enhanced respiratory protection and appropriate infection prevention and control measures are required to be fully and carefully implemented for all COVID-19 patients to reduce risk of aerosol transmission./
And concluding:
Appropriate PPE and mask use are essential as SARS-CoV-2 is frequently detectable in the airsurrounding positive patients. We believe our data supports the use of FFP2/3 medical masks for HCWs caring for COVID-19 patients, particularly for those with prolonged contact in line with HSE guidelines 15 289 . As we move forwards, we must continue to avoid oversimplifying the transmission dynamics of SARS-CoV-2 including into ‘droplet vs aerosol’, as this can lead to fixed IPC recommendations and must now appreciate that the ‘person, place and procedure’ influence transmission risk. Future recommendations must be guided by emerging evidence including ongoing studies to identify transmission differences that may occur with new variants of concern
In other words, Covid is pervasive, rather like background radiation. Covid really is airborne!
Conclusion
One asks why? Why would CDC promulgate, and HICCs accept, obvious falsehoods about airborne transmission, falsehoods that are obvious to anybody who keeps up with the literature? A parallel discussion of CDC’s documentation on ventilation in schools may provide a clue.
A week ago, I had a 2+ hour call with the senior engineers from CDC-NIOSH who are responsible for the content of CDC’s ventilation pages.(12/25)
— Devabhaktuni “Sri” Srikrishna (@sri_srikrishna) September 11, 2022
ACH (Air Changes for Hour) is a metric for ventilation:
(2) economic implications of putting these ACH numbers out there would cause “all hell to break loose” if well-meaning people across the country adopt them into building codes but later find out they cannot implement them with centralized HVAC systems. (16/25)
— Devabhaktuni “Sri” Srikrishna (@sri_srikrishna) September 11, 2022
Money! [slaps forehead][5]. Why didn’t I think of that? Also, of course, careerism, important to the PMC. So here we are.
NOTES
[1] Covid’s Most Vile Tweet™ is still up [pounds head on desk]:
FACT: #COVID19 is NOT airborne.
The #coronavirus is mainly transmitted through droplets generated when an infected person coughs, sneezes or speaks.
To protect yourself:
-keep 1m distance from others
-disinfect surfaces frequently
-wash/rub your 👐
-avoid touching your 👀👃👄 pic.twitter.com/fpkcpHAJx7— World Health Organization (WHO) (@WHO) March 28, 2020
4,340 quote-tweets, the last one fourteen minutes ago (as of this writing). So WHO is still damaging people’s health, good job,
[2] The United States seems, unbelievably, to be superior in mask protections to other “Five Eyes” countries, like the UK, Canada, and Australia, if the volume of outraged tweets is any indicator. Of course, in the US we may have just given up on outrage altogether, as with Covid generally.
[3] In the UK: “Transmission of SARS-CoV-2 to hospitalised patients likely caused approximately a fifth of identified cases of hospitalised COVID-19 in the “first wave” in England, but less than 1% of all infections in England.”
[4] The UK infection control community is as bad and possibly worse.
[5] I suggested the same in February 2021, based only on CDC documents [lambert preens].
APPENDIX: If Your Heatlh Care Facility Forces You to Remove Your N95
If you do not carry a Badger Frame (or Seal), here is a post on “How to Make a DIY N95 Mask” using a surgical mask and two eight-inch rubber bands.


